Defrosting Frozen Shoulder
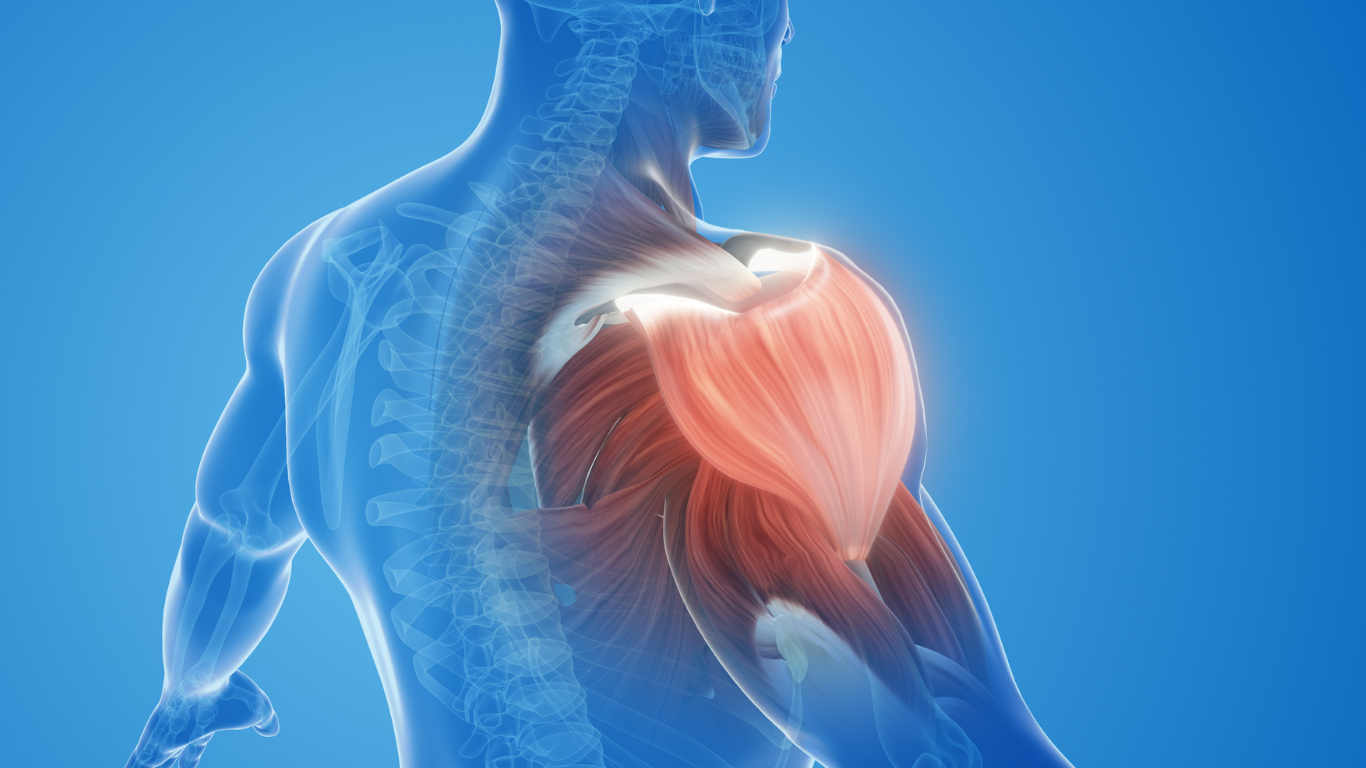
Posted on 28th October 2025 by Paul FrankhamFrozen shoulder, medically known as adhesive capsulitis, is a condition that causes pain and progressive stiffness in the shoulder joint, significantly impacting daily function and quality of life.
Despite its prevalence, it remains one of the most misunderstood musculoskeletal disorders. This blog aims to clarify the pathophysiology, clinical progression, diagnostic criteria, and evidence-based treatment strategies to provide clearer insight to patients and others interested in the condition.
Pathophysiology:
Frozen shoulder is characterised by:
- Fibrosis (scarring) and contracture of the glenohumeral joint capsule.
- Inflammatory synovitis (synovium – membrane lining of joints) leading to pain and restricted motion.
- Capsulo-ligamentous complex thickening, within the shoulder capsule.
There are two types:
- Primary (idiopathic): No known cause
- Secondary: Associated with trauma, surgery, or systemic disease- with the highest prevalence in those with diabetes or thyroid dysfunction.
Clinical Course:
Frozen shoulder typically progresses through four stages:
- Stage 1 – Pre-Adhesive (0–3 months)
- Sharp pain at end range of motion (ROM), achy pain at rest
- Sleep disturbances
- Early loss of external rotation
- Stage 2 – Freezing (3–9 months)
- Increasing pain and stiffness
- Loss of motion in all directions
- Synovitis and angiogenesis
- Stage 3 – Frozen (9–15 months)
- Persistent stiffness
- Pain may decrease
- Fibrosis of the capsule
- Stage 4 – Thawing (15–24 months)
- Gradual return of motion
- Pain resolves
- Residual stiffness may persist
Diagnosis:
Diagnosis is clinical and based on:
- Age: Typically affects individuals aged 40–65
- Gradual onset of pain and stiffness
- Restricted passive and active ROM, especially external rotation
- Pain at end-range movements
When consulting a physiotherapist, they will take a thorough history and conduct a clinical examination to confirm the condition’s features. If showing signs of these features, it is important to get a full physiotherapy assessment to:
- Rule out other conditions like rotator cuff tears, arthritis, or nerve entrapment, which can, in some instances, present similarly
Imaging may be recommended by a physiotherapist in some instances to exclude other pathologies, but it is not always necessary.
Treatment Guidelines:
Management is stage-specific, and physiotherapy will likely be dynamic based on your main symptoms and functional limitations:
Your Physiotherapist may ask you to fill out a questionnaire with questions about the effort level required to perform everyday tasks and whether you experience any pain or issues during their performance. These will help highlight functional limitations that you can work together with your physio to address.
Furthermore, after assessment, your physiotherapist may describe your shoulder as a ‘Painful shoulder’ or ‘Stiff shoulder’, and treatment choices will likely differ depending on this.
Firstly, treatment will begin with Education regarding your condition:
- Reassurance- ‘serious underlying causes of shoulder pain are rare, and the condition is generally self-limiting with a natural course
- Acknowledgement and education regarding the spectrum of symptoms and severity
- Avoidance of immobilisation
- Teaching activity modifications to reduce symptom aggravation, for example:
Dressing – wearing loose, front-fastening tops. Inserting the affected arm into clothing first
Lying/prolonged arm posture – utilising proper support, such as pillows or rolled towels, can improve comfort and reduce strain.
‘Painful Shoulder’
Those presenting with high symptoms of irritability will generally combine physiotherapy with other treatment modalities.
A Cochrane study concludes that there is “little overall evidence to support physiotherapy treatment alone in the treatment of Frozen Shoulder”
To better control pain, modalities such as heat, ice and electrical stimulation may be utilised to increase comfort. Your physiotherapist may also advise you to start taking Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) to aid your ability to perform exercise and daily tasks.
You may also be referred to an orthopaedic doctor with a view to getting a corticosteroid injection.
Based on a network of nine studies, the MTC found that steroid combined with physiotherapy was the only treatment showing a statistically and clinically significant beneficial treatment effect compared with placebo for short-term pain.
Cochrane Review:
Pain: Manual Therapy and exercise are not as effective as glucocorticoid injection
Function: Patients with Manual therapy and exercise did not improve as much as glucocorticoid injection
- 46/100 reported treatment success with manual therapy and exercise
- 77/100 reported success with steroid injection = 31% improvement
(Page et al., 2014)
Gentle manual treatment to help improve comfort will also commence:
- Therapist-assisted passive ROM (PROM) exercises
- Gentle Shoulder mobilisation (glides)
- Gentle Soft tissue work around the neck, shoulder or scapular muscle release
Home exercise will also be an important treatment to protect joint range and to desensitise pain:
- Pendular exercises, which involve gentle gravity-assisted oscillatory movements, can help downregulate pain and promote gentle movement of the shoulder capsule
- Passive and assisted exercises using equipment such as a pulley can also induce gentle movement
- All should be held for Short-duration (1–5 seconds) and within relatively pain-free ranges
K tape may also be trialled with its ability to help reduce pain and to support more ‘normal’ shoulder and scapula movement
‘Stiff shoulder’
As the course of the condition progresses, pain should reduce, and stiffness of the shoulder generally becomes more prevalent. You should experience lessened symptom irritability at this time.
The above treatments can still be utilised, but now progression can be made to increase the motion and function of the shoulder joint.
Manual therapy:
- Progression of Mobilisations with higher amplitude and towards end of range to help improve range of movement
- Scapular mobilisations to help with overhead activity and promote normal scapulohumeral movement patterns
- Continuation of soft tissue work around the neck, shoulder or scapular muscle release
- Proprioceptive Neuromuscular Facilitation (PNF) involves specific movement patterns combined with manual resistance, stretching, and isometric contractions. These patterns mimic functional movements and stimulate proprioceptors to improve muscle activation and joint mobility.
- Therapist-assisted stretches to increase shoulder range and function:
Examples – Sleeper stretch (improve shoulder internal rotation) and cross-body stretch (Stretch posterior shoulder capsule)
Home Exercise: Introduction of strengthening exercises
Beginning:
- Isometric (static contractions) shoulder exercises and rotator cuff work
- Light scapula and upper back exercises
- Shoulder capsule stretching – within tolerable levels (15s or less)
Later:
Progressions to high-demand functional and/or recreational activities
- Strengthening work (resistance bands, free weight and machine) – (Target rotator cuff strength, deltoid and chest, lats and scapular)
- Stretching: Emphasis on mobility exercises and stretches towards end of range (holding longer duration ≥30 s)
- Guiding return to normal activities and hobbies
Conclusion:
Frozen shoulder is a self-limiting condition, but its impact on function and quality of life can be profound. Early diagnosis and stage-appropriate physiotherapy interventions are key to optimising recovery. With a structured approach, most patients regain near-normal shoulder function over time.
References:
Page, M.J., Green, S., Kramer, S., Johnston, R.V., McBain, B., Chau, M. and Buchbinder, R. (2014). Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database of Systematic Reviews, (8). doi:https://doi.org/10.1002/14651858.cd011275



