What is boom and bust, and how can it be avoided?
We have mentioned the boom-bust mistake you could make if you’re a weekend warrior or were overly enthusiastic about your health-related new year’s resolutions. So what is boom-bust & what’s wrong with it??
When we say boom-bust we mean drastically changing your fitness routine, way of life, or habit from what you were doing previously, only for it to go wrong and you give it all up again- whether that’s because of lack of dedication or succumbing to injury. If this happens it probably means you took on too much, too soon & overwhelmed your system.
Significantly changing your lifestyle and exercise regime can be exciting but can easily lead to injury from overloading soft tissues or joints, especially if there’s not enough rest or recovery between sessions. This loading is scientifically investigated by researchers who call it the acute to chronic workload ratio- acute workload being what session (or sessions) you do today, and chronic workload being the summation of these sessions over a week or month. There’s a sweet spot in the ratio which means you can gradually increase your training with much less risk of injury, though if you go under or over this sweet spot then you’re either not gaining anything from your training, or you’re at high risk of injury (boom) which halts your training & leaves you feeling dejected (bust).
We’ll go into more detail on the acute to chronic workload ratio in another blog post, showing how you can use it to train smarter and aim to avoid injury.
For now, we’ll say try to change one thing at a time and keep the changes gradual, here are some examples of how you can achieve this:
- Incorporate rest or recovery days between workout days; instead of doing a HIIT workout every morning swap two workouts per week for mobility, low-key yoga or meditation.
- If you’re new to running then try following the NHS Couch to 5K programme, an awesome way to get into running without biting off more than you can chew.
- Focus on active recovery- by this we mean taking the time to unwind & enjoy a hot bath, spending 10 minutes foam rolling or stretching any areas which have caught your attention, fitting in a power nap, or booking in that sports massage you’ve been meaning to have for the past year!
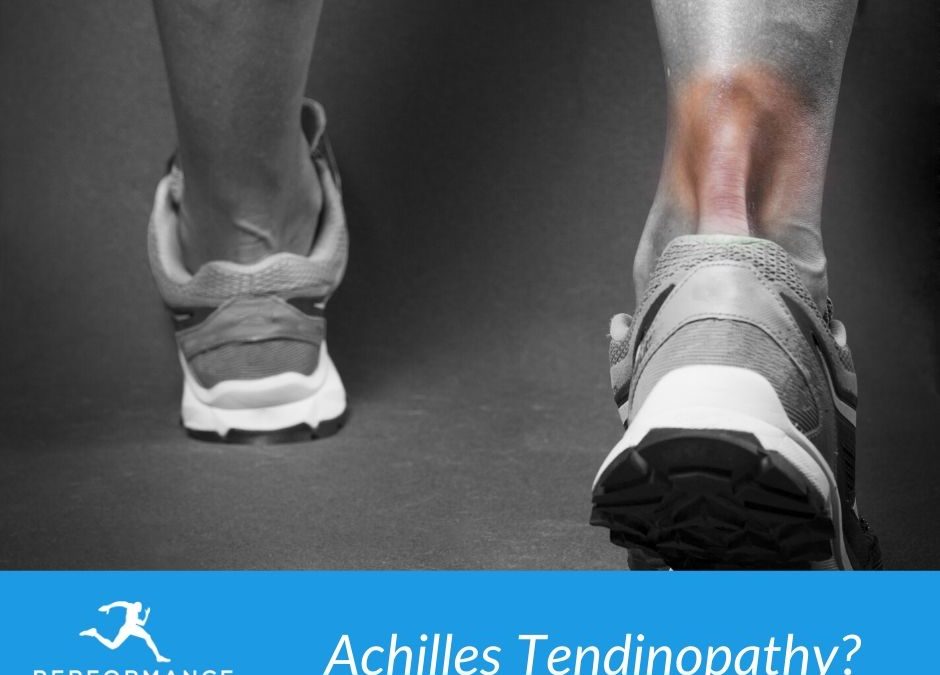
- Listen to your body- if you’re dragging your knuckles because you’re tired and feeling run down then maybe today’s the day to swap the cliffpath run you’d been planning for an easy stroll or light stretch. If there are any bodily areas that consistently get your attention then it’s probably worth booking in with a physiotherapist who’s experienced in assessing these issues and checking it’s not becoming something concerning.
- Keep a diary or log of what you’re planning to do, and then record what you’ve actually done. It’s easy to get carried away in the momentum & enthusiasm though if you’ve got a record of it, it will be easier to see where you’ve gone wrong and prevent it from happening again.
Hopefully, that’s given you some food for thought, be kind to yourself and your body and you never know what you’ll achieve!